What is bronchiectasis?
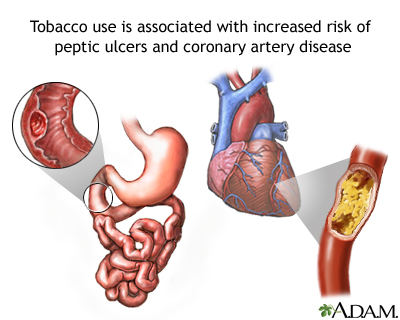
Bronchiectasis is a lesser known, but equally common lung disorder. With bronchiectasis, a person develops large, swollen, and inflamed airways which make copious secretions and cause a chronic cough. Sometimes, there is thick, sticky mucus. Sometimes, just a harsh and chronic cough is presents. Just as with other lung diseases, mucus production and cough are usually our first line of defense against infection and irritants. The most common irritants that cause this problem are tobacco smoke and heartburn.
Heartburn is more accurately referred to as reflux, as there is not always a burning sensation if the stomach contents are not very acidic. This stomach material comes up the esophagus or food pipe, and then slips back down the trachea or windpipe, as both pipes open into the back of the throat. You will realize this if you think about what happens when you drink something and it “goes down the wrong pipe” and makes you choke. Stomach contents are very irritating to the lung and cause the airways to become quite inflamed.
Another irritant which is particularly damaging, although less commonly seen, is oil. When fatty or oily material gets into the lung, the lung cannot clean it (“like oil in water”) and permanent damage can occur. Most people will never get oil into their lungs, however, there are people who will put oil-based creams and ointments into their nasal passages for dryness or congestion. These products are usually labeled “for external use only” but many people do not consider the inside of the nose to be “internal,” since they are not swallowing it. As the nasal passages warm the material, it becomes a liquid and runs down the nose into the lung, during wake and especially during sleep, when the head is tilted back. This is one of the worst materials one can directly put into the lung.
Please remember, you should never put anything into your nose which is not a nasal spray. Another possible oily source is peanuts. It is difficult to understand why people throw things into the air and try to catch them in their mouths. If they have good aim, it will travel straight down the throat and into the lungs. This can lead to pneumonia, and sometimes a camera must be placed into the lungs to try and remove this “foreign body.” In the worst-case scenario, surgery may be required to remove the object and damaged lung.
What can be done to treat bronchiectasis?
There are several ways to treat the irritation and swelling of the airways. First, stop the irritant. Smoking and oily products must be avoided. Reflux must be aggressively treated. When it reaches this level of severity, i.e., lung damage, then it is important that a specialist or gastroenterologist be involved. Some patients may have their reflux controlled with lifestyle or medications, others may require endoscopic procedures or surgeries. The second step is to control the mucus production. The mucus that is usually created with this condition is thick and difficult to expectorate. Treatments are aimed at thinning secretions and improving expectoration, which is also known as pulmonary toilet. To thin the secretions, medications called mucolytics are used, and include decongestants and inhaled medications which “loosen” the phlegm. There are multiple techniques used to improve expectoration. Chest percussion and vibration, either manually or with devices, is usually the procedure of choice. This is usually performed after administering the mucolytic, so that the phlegm is easier to dislodge. In a loving relationship, your spouse can learn how to percuss the back of the chest to augment coughing. If percussion is to be self-administered, devices such as a flutter valve, vest percussor device, or intermittent positive pressure device with a mouthpiece can be used. The goal is to bring up as much sputum as possible and cough or spit it out.
Finally, as with other lung diseases, control of inflammation is also important. Frequently, inhaled steroids are used to improve inflammation as in other pulmonary illnesses previously described. It is important to immediately see the doctor when sputum has changed color or increased amount, even if you don’t feel short of breath or don’t have a fever. This may be an early sign of increasing inflammation or infection and should be treated promptly. You should also avoid any sick family or friends and only visit when they are well.
We could not leave a discussion of bronchiectasis without mentioning infection. These swollen airways can easily and frequently become colonized with bacteria and infected. Colonization means that the bug is alive and growing in the airways, but it is not causing any damage or making you sick. Infection means that the bug is alive and growing in the airways, and that it is causing illness or disease. One of the most common bacteria found in patients with bronchiectasis is pseudomonas. It particularly likes patients with cystic fibrosis. It has been increasingly recognized that cystic fibrosis may include a large spectrum of illnesses, ranging from a severe childhood illness to recurrent cough in adults with bronchiectasis. It can be managed with antibiotics, but if cystic fibrosis is contributing to the illness treatments specifically aimed at this disorder should be applied. A second infection is more common in older, slender women. This infection is due to Mycobacterium avium intracellulare, also known as MAI, not to be confused with its cousin, Mycobacterium tuberculosis, or M.TB. There have been several guidelines published to help distinguish whether MAI is a colonizer or causing infections in patients. Unfortunately, many of the treatment options for MAI include multiple medications for a prolonged period. Patients can remain on medications for this infection for 12 months or more. Finally, the last bacteria that is commonly found in the airways of patients with bronchiectasis is methicillin- resistant staphylococcus aureus or MRSA. This infection is commonly seen in people who have had several hospital visits or have stayed in a facility, such as a nursing home or rehabilitation center. Just like other bacteria, it can be a colonizer or cause infections. While infections with these organisms can usually be treated, it is often difficult to eradicate and get rid of them entirely and they can progress to pneumonia.
What happens if I start to cough blood?
There is a very close relationship between airways and blood vessels because the main job of the lungs is to bring air into the bloodstream. In patients with bronchiectasis, the airways are enlarged and sometimes erode into the blood vessels or become inflamed in bleed easily. It is common when there is increased inflammation or infection for someone with this disorder to start coughing blood. When this happens, you should seek medical attention right away.
What tests are commonly used to evaluate bronchiectasis?
The first test usually done is a high-resolution CAT scan of the chest to evaluate the size of the airways and look for other lung diseases, as well as a pulmonary function test. Other tests may include blood work to check the immune function and screen for cystic fibrosis. If your immune function is poor, you may require chronic iv treatments to support your immune system. Tests to evaluate for gastric reflux or heartburn as well as swallowing disorders may also be performed. Tests may also be done to evaluate for chronic infection, including sputum cultures or bronchoscopy.
Will I need surgery to treat my bronchiectasis?
Very rarely, people may need surgery to treat bronchiectasis, either to control bleeding or help to treat chronic infection in damaged lung tissue.
Self-Check for Management of Bronchiectasis
- I have had a complete evaluation of my bronchiectasis and know why my airways are swollen. I know what future irritants to avoid.
- I know what medications I need to keep the inflammation down, relieve cough and decrease mucus production.
- I receive my vaccinations as needed to prevent lung infections.
- If my sputum changes color, increases in amount or becomes bloody, I know to call my doctor and be further evaluated for infection.
Managing Doctors
- Primary care
- Pulmonary
- Gastrointestinal (GI)
- Ears, Nose, Throat (ENT)
- Allergy / Immunology