What is asthma?
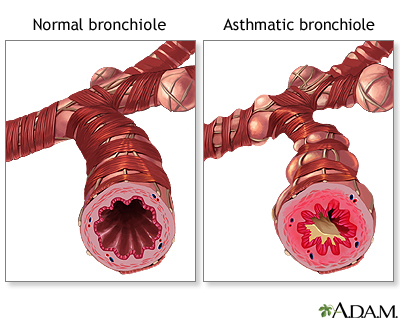
Asthma is similar to COPD since there is airway constriction and obstruction to airflow. But unlike COPD, asthma usually involves inflammation and constriction of mainly the small airways. It is felt that asthma is due to irritants that enter the lung, but there is also felt to be a strong immunologic etiology as well. This reaction to irritants may be nature’s way of telling us to avoid things which are bad for the lungs. Ironically, avoidance of irritants is one of the cornerstones of asthma management. Asthma symptoms can include any one or more of the following: shortness of breath, wheezing, chest tightness, or cough.
As far as the overall illness goes, asthmatics have two phases of illness, chronic inflammation, and acute bronchospasm or constriction. Asthmatics are much more sensitive to acute and chronic inflammation, and higher and more chronic doses of inhaled steroids are frequently used. Sometimes, these are augmented by other anti-allergy medications, such as leukotriene inhibitors and antihistamines, which happen to be particularly effective for people whose asthma is provoked by exercise. If a patient has heartburn, the acid from the heartburn is also a strong lung irritant.
Can I get asthma if I didn’t have it as a child?
Yes. Asthma can be diagnosed as any age.
Will my asthma ever go away?
Asthma that develops during childhood or during pregnancy, may resolve in time. People who develop asthma as an adult usually continue to experience asthma symptoms.
What is the best initial treatment of asthma?
The key initial step to asthma management is avoidance of triggers. If you know what will trigger your asthma, you should avoid it. For example, smoke, perfume, cold air, dust, and pets are common triggers. Now I happen to be an animal lover, so I understand when people tell me that their cat isn’t going anywhere, despite their asthma, I can be a little flexible. This can be tolerated under a few conditions. First, there is an understanding that the cat will make your symptoms worse. Not necessarily because of the cat dander, but because of everything they are leaning against and “dusting” as they walk around your home, no matter how clean it is. They are bringing this directly to you. Second, the cat must be out of the bedroom. Cat dander and the associated irritants in the fur will get onto you bed and will be in direct contact with your nose/mouth (aka airways and lungs) the entire time you are sleeping (i.e., 5-8 hrs.). Third, you must religiously take your medications and stay on top of your asthma. Finally, if there are several hospitalizations for asthma, or you end up in the Intensive Care Unit, then “Fifi” is moving in with the relatives.
If exercise triggers your asthma, using medications and having a warm-up period prior to maximal exercise may greatly reduce your symptoms. By the same token, if cold air triggers symptoms, using medications prior to exposure to the cold and wearing a scarf about the nose and mouth may also help to decrease symptoms.
What allergen control methods work?
On the same note, there is a big market for allergen control products, and some are endorsed by different societies and have all kinds of seals of approval. I recommend that you stick to cheap and effective. Clean frequently and with soap and water. If you are using sprays to clean with, make sure that the room is well-ventilated (i.e., windows open). Change the filters on your air conditioner weekly to monthly (depending on the allergen load) and have your heater serviced regularly. Also, you should buy a carbon monoxide and smoke detector. If you want to use special devices, I recommend a. HEPA (high efficiency particulate air) filter. You should avoid any device that makes or uses ozone, as this may make your asthma worse. Interestingly, house plants, such as Ivy, may be just as effective at cleaning the air.
What medications are used to treat asthma?
There are two types of medications used to treat asthma. The “control” medications are used to keep inflammation and allergy under control. This group usually includes the inhaled steroids, decongestants or antihistamines, and leukotriene inhibitors. These medications are taken every day to keep asthma controlled and to prevent attacks. There is also an injected medication called omalizumab, which is sometimes used for severe allergic asthma.
The second group of medications are the “rescue” medications, used to treat the symptoms of asthma. These are the bronchodilators, which are medications used to prevent constriction and open the airways or ‘”bronchioles.” These medications sometimes cause patients to feel like their heart is racing or feel anxious or jittery. This feeling can sometimes be reduced by reducing the dose of the medication, changing the timing, or eating a banana with it.
What is the difference between an inhaler and a nebulizer?
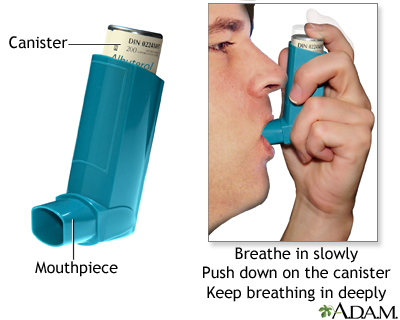
The term “inhaler” or metered-dose inhaler refers to a drug delivery device that aerosolizes medication via a handheld spray into small droplets that can be inhaled or breathed into the lung. Large droplets would be swallowed, while droplets that are too small will be inhaled and exhaled (like air). Therefore, the dose is measured or “metered” to be just the right size and amount. Inhalers are most effectively used with a plastic tube called a “spacer” or chamber. This allows the spray to be a mist before it is inhaled, so that all the medication is airborne and then inhaled, instead to squirted on all the surfaces of the mouth and lost. Powder inhalers do not require a spacer like the liquid ones do. You must take a strong breath in, and the powder is very light and immediately airborne.
However, if you cannot take a strong and fast breath in, you will also not get all the medication and may need to switch to either a liquid inhaler or a nebulizer. When you correctly use an inhaler, you may not feel or taste the medication, as it all gets brought directly into the lung. Inhalers should last about a month, and if you are using more than one canister of medication per month, you should talk to your doctor. By the same token, if you rarely use a medication, be sure that you renew and refill it when it expires, or when you use it you may not have active drug. The usual routine for inhaler use is as follows: inhaler is primed and attached to the spacer, shake the inhaler, hold the spacer to the lips, exhale, depress the inhaler and the spray or mist enters the chamber, take a deep breath in, hold breath for a count of 10 (or best you can), exhale, wait a minute, then take the next puff of medication in the same way. Repeat for the number of puffs you are prescribed. If you are using an inhaled steroid, rinse your mouth well immediately after use. You should have your doctor or respiratory therapist watch you use your inhaler to be sure that you are using it correctly.
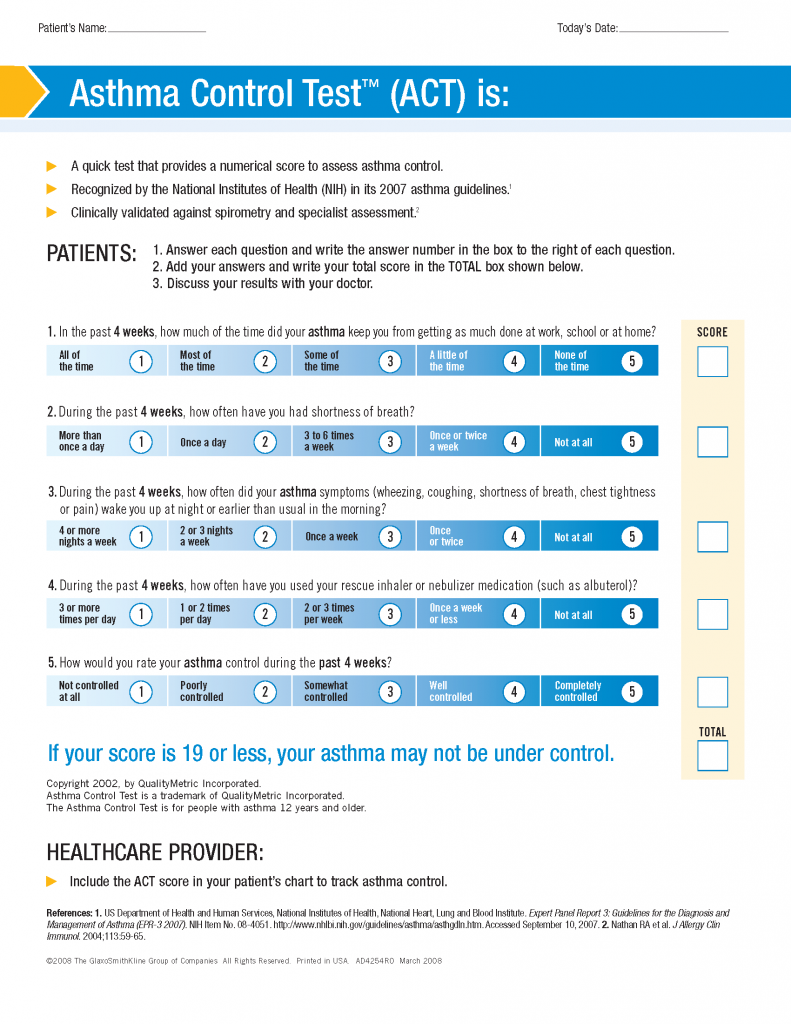
How do I know if my asthma is well-controlled?
There are several ways to know that your asthma is being well-controlled. You can review an “Asthma Control Test” questionnaire with your doctor, which reviews your asthma symptoms and inhaler use, to see how good your control is, and if it is improving or worsening. Some signs of poor asthma control include frequent inhaler use, waking up at night with symptoms, frequently needing steroids, having multiple ER visits a year, and being hospitalized due to asthma.
What is an asthma attack?
Asthma attacks happen when an irritant or infection causes your asthma symptoms to suddenly appear, and you need immediate medication for relief and restoration of normal breathing. Small airway size is regulated mainly by the sympathetic or “beta” system. Beta-agonists are medications which promote the opening of the small airways, “rescue medications.” Just a note, it is best to have more than one rescue inhaler, so that you can leave one in different locations for emergencies, such as work, school, the car, gym or bedroom. In this way, you never have to go too far to get an inhaler when you really need it.
You use this information and your symptoms to make a written asthma action plan with your doctor. It provides treatment instructions of what medications to take for a mild, moderate, or severe attack of your asthma. It will instruct you on when you can adjust your medications yourself, when need to call the doctor, and when you need to go to the Emergency Room or call 911. The dosing of your medications on an asthma action plan may be higher than you usually take.
What is meant by life-threatening asthma?
All asthma has the potential of being life-threatening. Danger signs that your asthma is out of control include: running out of your medications, frequent use of your rescue inhaler, not having relief after using your inhaler, and frequently requiring steroid tablets to keep your asthma under control.
Are there any experimental/surgical treatments for asthma?
There is a new procedure called bronchial thermoplasty. A camera is placed into the airways while you are asleep/sedated. Heat is used to burn/reduce muscular tissue, which limits the amount it can restrict/close shut during an attack.
What routine testing / monitoring may be done to evaluate my asthma?
Common tests which are performed include a peak expiratory flow rate, pulmonary function test and CXR. Other tests may include blood work, such as immunoglobulin levels, eosinophil level, screening for Aspergillus or screening for vasculitis. An echocardiogram or CAT scan of the chest may also be performed. If there is chronic sputum production, sputum may also be tested. Patients may also have a CAT scan of the sinuses or further evaluation for reflux or swallowing disorders.
Self-Check for Management of Asthma
- I have made a list of my common asthma triggers and have planned for better ways to avoid them.
- I understand the difference between control medications and rescue medications. I have a list of my medications and how to use them.
- I understand how to use inhalers or nebulizers correctly and have an asthma action plan. My family/friends and co-workers know what to do if I have an asthma attack.
- I keep my asthma medications handy and do not use expired medications.
- I keep my vaccinations up to date to prevent lung infections.
Managing Doctors
- Primary Care
- Pulmonary
- Allergy or Immunology
- Gastrointestinal (GI)
- Ears, Nose, Throat (ENT)